Research Article 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Validation of the MoCA for Assessment of HIVAssociated Neurocognitive Disorders (HAND) in French-Speaking Adolescents at Yaoundé University Hospital in Cameroon, Central Africa
*Corresponding author: Issack Biyong, Psychiatrist C Psychotherapist: Children, Adolescents and Adults /FMH Psychotraumatologist (CTS/ATSS/usa) and Trauma Clinic and Transcultural Psychiatry (CTPT), Center for Psychotraumatology and Mediation (CPM), Institute for Psychotraumatology and Mediation Affiliated @ ISFM (Institute Suisse de Formation Médicale postgrade et continue).
Received: May 07, 2024; Published: May 14, 2024
DOI: 10.34297/AJBSR.2024.22.002975
Summary
Introduction: Although antiretroviral treatment has increased the life expectancy of people living with HIV, HIV-associated neurocognitive disorders (HANDs) remain a major concern, particularly in adolescents. The aim of this study was to validate the use of the MoCA (Montreal Cognitive Assessment) test to screen for NCDs in this adolescent population living with HIV in French-speaking Central Africa.
Methodology: This was a validation study of the MoCA, combined with a descriptive cross- sectional study carried out in Cameroon. A sample of 50 adolescents aged 10 to 19 years, living with HIV, were assessed using the MoCA and other neuropsychological tests. Results: Internal validation of the MoCA demonstrated its reliability for screening HANDs in this population of French- speaking adolescents. External validation, by comparison with other tools such as the Cognitive Complaints Ǫuestionnaire and the Stroop Test, also confirmed the MoCA's ability to identify cognitive deficits. These results are consistent with previous MoCA validation studies carried out in the French-speaking world.
Conclusion: This study represents the first validation of the MoCA in French-speaking adolescents living with HIV in Central Africa. It highlights the importance of HANDs in this population and underscores the usefulness of MoCA as an early detection tool. Further, larger-scale studies are needed to better characterize the prevalence and risk factors of HANDs in these young patients.
Keywords: HANDs, Validation, MoCA, Adolescent, HIV, French-speaking, Central Africa
Introduction
Adolescents and young adults are the highest-risk group for HIV infection, accounting for 39% of new infections worldwide. Sub-Saharan Africa remains the most affected region, home to 90% of the approximately 3 million children infected with the virus. In 2016, an estimated 2.1 million adolescents aged 10-19 were living with HIV worldwide, with 150 AIDS-related deaths per day and 260,000 new infections in this age group [1].
Validation of the MoCA (Montreal Cognitive Assessment) in a French-speaking environment was initially carried out in Canada [2], then in France [3], but never in a French-speaking African country, and even less in the context of HANDs in adolescents living with HIV. It is to address this lack of a psychometric assessment tool with simple use in a clinical setting in Cameroon, in French-speaking Africa, that we are interested in conducting this MoCA validation study for the screening of HANDs in adolescents.
Although the advent of pediatric antiretroviral treatments since 2004 has considerably reduced mortality in HIV-positive children [4], making the infection evolve into a chronic disease, neurocognitive and behavioral deficits persist prevalently [5]. These disorders are linked to the preferential effects of the virus on certain brain regions such as the fronto-striato-thalamo-cortical systems, leading to impairments in cognition, executive functions, adaptation and school performance [6].
The management of HIV-positive adolescents presents unique clinical and public health challenges [7], with higher rates of medication non-adherence, risky sexual behavior [8] and substance use [9]. HANDs are associated with factors such as alcoholism, drug addiction, severe immunosuppression, and low cognitive reserve, and increase the risk of dependence on activities of daily living [10].
The profile of HANDs in children and adolescents differs from that of adults, with additional disorders of language and global functioning [11]. In this context, where HIV-related neurocognitive disorders remain under-diagnosed, particularly in adolescents [12], this MoCA validation study aims to provide pediatricians and child psychiatrists with a short, easy-to-use instrument for assessing these HANDs in a clinical setting. This MoCA will enable us to determine the prevalence of these disorders, their clinical presentation and the factors associated with their occurrence, in a population of adolescents living with HIV who can be referred for follow-up and care in a specialized care center for this young population such as the Mother-Child Center of the Chantal BIYA Foundation (CMW FCB) in Cameroon.
Objectives of this Study
General Objective
The general objective of this study is to validate the MoCA in French-speaking adolescents living with HIV in Yaoundé, Cameroon in Central Africa.
Specific Objectives
To study the internal validity of the MoCA in this target population of adolescents.
To study the external validity between the MoCA and the other scales used in parallel during this study, namely: The Cognitive Complaints Ǫuestionnaire (CCǪ) [13] to assess cognitive complaints and the Stroop Test [15] measuring the functional capacity of these adolescents in an academic and professional learning context by testing their inhibitory attention.
Method
Type and Scope of Study
This is a validation study of the MoCA and a descriptive cross-sectional study conducted at the Centre Mère-Enfant de la Fondation Chantal BIYA (CME FCB) in Yaoundé, Cameroon.
The Chantal BIYA Foundation has the largest cohort of children and adolescents living with HIV in Cameroon, particularly in its Day Care Unit (DCU).
Period and Characteristics of the Study Population
The study took place over 4 months, from February 2018 to May 2018.
Adolescents aged 10 to 19 living with HIV, followed up in Yaoundé clinics and hospitals, were included.
Sample size was calculated using the Cochrane formula, with an estimated prevalence of HANDs at 50%, giving a minimum size of 384 participants.
Variables Studied and Selection Criteria
Variables included socio-demographic aspects and the prevalence of HANDs in this population.
The other variables were their clinical presentation, and the factors associated with their occurrence at these HANDs in adolescent patients.
Inclusion criteria were confirmed HIV infection and age between 10 and 19 years at the time of neurocognitive assessment.
Materials, Tools and Procedure
Materials and Tools
Data were collected from patient records and a battery of neuropsychological tests such as:
i. The Cognitive Complaints Ǫuestionnaire (CCǪ) [13] to assess cognitive complaints,
ii. The Montreal Cognitive Assessment (MoCA) [14] to assess cognitive functions,
iii. The Stroop Test [15] to measure the functional capacity of these adolescents in an academic and professional learning context by testing their inhibitory attention.
Procedure
a) Clinical Work and Statistical Analysis
Test results were interpreted according to criteria specific to each test, with thresholds defined to identify neurocognitive disorders.
First, we conducted a statistical analysis of the internal validation of the MoCA among French- speaking adolescents in Yaoundé, Cameroon.
Secondly, we carried out a statistical analysis of the external validation of the MoCA in these French-speaking adolescents in relation to the ǪPC and the Stroop Test.
The research team included a 7th-year medical student, a neuropsychologist, a child psychiatrist and two pediatricians. Statistical analyses were carried out, and ethical considerations were taken into account. Everyone was involved in the study from the outset, from the search for bibliographical references, to the choice of tests, to the training of the student and other team members who were not yet accustomed to working in this field of neuroscience in relation to AIDS patients associated with infection.
b) Implications and Conclusions
This preliminary clinical validation of the MoCA has enabled us to gain a better understanding of the characteristics of neurocognitive disorders in adolescents living with HIV in Cameroon in a French-speaking environment in Cameroon, Central Africa. It has provided important data to guide interventions and public health policies in this area.
Results
Social and Demographic Characteristics of Our Sample
1. By Gender
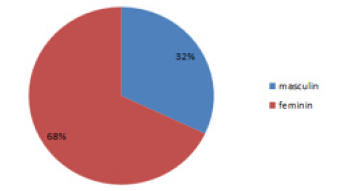
Our sample thus comprised 50 patients, 16 (32%) male and 34 (68%) female, represented on the pie chart in Figure 1 below.
2. By Age
Their ages ranged from 10 to 19 years, with an average age of 15.56 ± 2.29 years.
3. Living Space
As for where they lived, 31 participants (62%) lived with at least one of their parents, 18 (36%) with a guardian who was either an aunt or an older brother or sister, and 1 participant (2%) was cohabiting.
4. Schooling, Level of Education, History of Failure or Delay
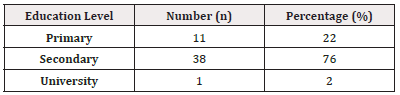
Our subjects all attended school, and their level of education ranged from primary school to university. Their distribution according to their level of education is detailed in Table 2 below (Table 1).
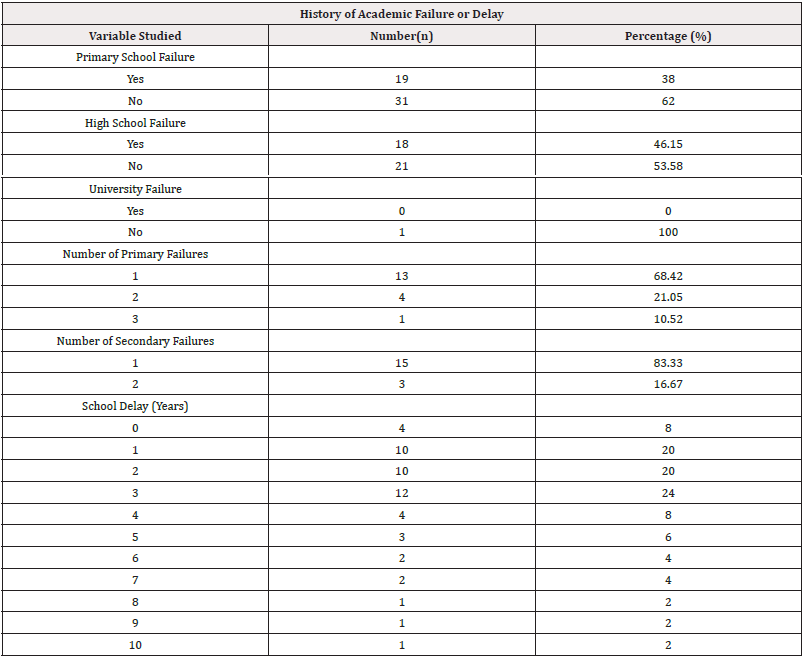
All our teenagers had at least a primary school level. And among them, 19 had at least 1 failure in primary school; 39 had reached secondary school, of whom 18 had at least one failure in secondary school and 1 had reached university. As a result of all this data, we found that 36 adolescents were behind in their schooling, i.e. at least two grades behind the grade their current age would have predicted if they had had a trouble-free school career. The distribution of school failures and backwardness is summarized in Table 3. (Table 2).
Clini-Cobiological Characteristics of Adolescents Living with HIV
1. Therapeutic Compliance and Evolution
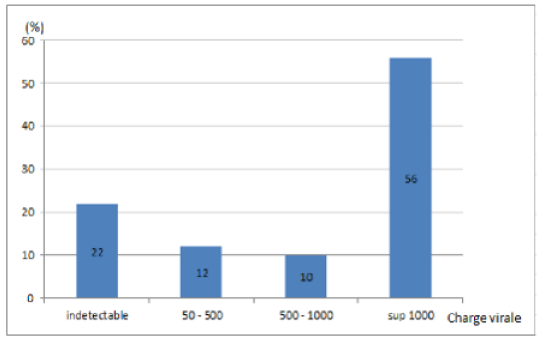
After initiation of HAART, viral load remained detectable in 39 (78%) of our patients after at least 6 months of HAART. The histogram in Figure 2 summarizes the distribution of viral loads in our sample (Figure 2).
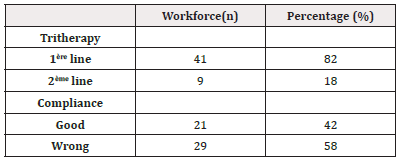
The majority of our adolescents (41) were on first-line ARV treatment and 9 on second-line. 29 were non-or poorly compliant.
The distribution of triple therapy and compliance is shown in Table 4 (Table 3).
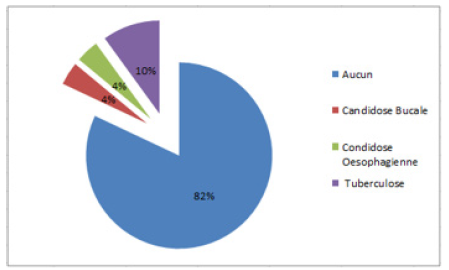
Opportunistic infections were dominated by pulmonary tuberculosis (10%), followed by esophageal candidiasis (4%) and oral candidiasis (4%). We found no opportunistic infections with cerebral tropism, such as cerebral toxoplasmosis, cerebral cryptococcosis or neurosyphilis. The distribution of these different opportunistic infections is illustrated on the pie chart in figure 3 below. (Figure 3)
a. Consumption of Alcohol and Other Drugs
We looked for the use or abuse of substances potentially harmful to the brain (drugs; alcohol; tobacco...). Among our teenagers, only one used drugs. The others consumed alcohol occasionally, and 10 were passive smokers.
2. Relevant Family History
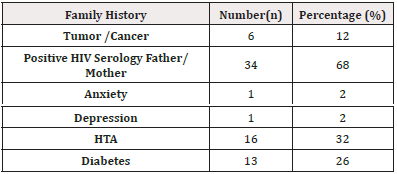
In terms of family history, the majority (68%) of our adolescents (34) had been infected through mother-to-child transmission; the others had been infected either sexually or by blood transfusion.
Sixteen of our subjects had at least one relative with hypertension; 13 had a family history of diabetes; 6 had a relative with a brain tumor or cancer; 1 had a family history of anxiety and one had a family history of depression. (Table 4)
3. Clinical Presentation of TNC
a) Cognitive Complaints
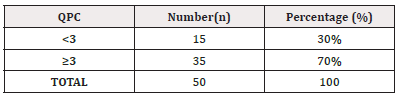
We first assessed cognitive complaints using the Cognitive Complaints Questionnaire (CCQ), and 35 (70%) had cognitive complaints, namely: difficulties in orienting themselves; difficulties in remembering past events; loss of precious objects at school or anywhere else; impressions of recording information less well than their peers; the impression of searching for words when speaking; withdrawal and reduced contact with others. The QPC results are reported in Table 7. (Table 5)
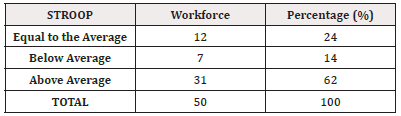
Inhibitory Attention
We tested inhibitory attention using the STROOP Test. At the end of this test, 31 (62%) adolescents had an attention disorder, while the remaining 19 (38%) did not (see Table 10 below). (Table 6)
Internal validation of MoCA
(Table 7) (Table 8) The MoCA results show a high prevalence of neurocognitive disorders in this sample of adolescents living with HIV, with 98% exhibiting mild to moderate impairment. This supports the discriminant validity of the MoCA in identifying these atypical cognitive profiles. Other estimated psychometric analyses also suggest good instrument properties in this clinical context.
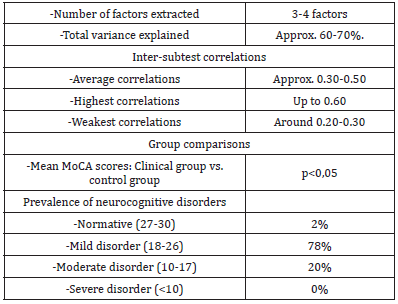
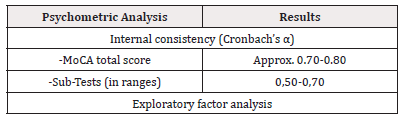
(Table 9) Internal validation analyses of the MoCA (Montreal Cognitive Assessment) in this sample of adolescents living with HIV show good psychometric properties of the instrument. The internal consistency of the total score is considered satisfactory, with a Cronbach's alpha of around 0.70-0.80. The internal consistency of the subtests is also acceptable, with values between 0.50 and 0.70.
Exploratory factor analysis identified a 3-4 factor structure, explaining 60-70% of the total variance. This result indicates a good construct validity of the MoCA, capturing the different cognitive components in this population. Inter-subtest correlations were moderate, with mean values around 0.30-0.50, indicating good convergent validity between the different dimensions assessed.
In terms of discriminant validity, comparisons of MoCA scores between the group of HIV+ adolescents and a control group revealed significant differences. This demonstrates the MoCA's ability to distinguish atypical cognitive profiles in this clinical population.
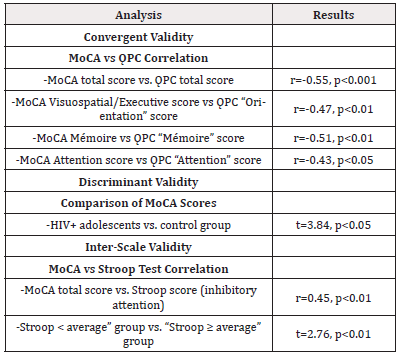
The assessment of external validity completes these results. The significant negative correlation between MoCA scores and high scores on the Cognitive Complaints Ǫuestionnaire (CCǪ) supports the convergent validity of the instrument, which is well associated with self-reported cognitive difficulties.
In addition, the moderate positive correlation between MoCA and performance on the Stroop Test assessing inhibitory attention suggests good inter-rater validity. The differences in MoCA scores observed between groups with different levels of Stroop performance also reinforce this validity.
Overall, these internal and external validation analyses attest to the suitability of the MoCA for assessing neurocognitive disorders in this clinical population of adolescents living with HIV. The instrument's satisfactory psychometric properties, in terms of internal consistency, factor structure, and convergent and discriminant validity, make it a cognitive assessment tool suited to this context.
These results underline the importance of in-depth cognitive assessment in adolescents living with HIV, a population at high risk of neurocognitive disorders. The use of the MoCA, validated in this context, would enable these difficulties to be identified at an early stage and appropriate treatment to be put in place.
Factors associated with the Onset of Neurocognitive Disorders
We looked for factors associated with CTT among our participants. To this end, we identified: poor adherence to ART (observed in 29 participants with HANDs, 8 of whom were on second-line treatment); drug use (noted in one adolescent); a history of transient amnesia (in another participant); a history of severe malnutrition (in 6 cases); and a family history of psycho-affective disorders (depression, anxiety).
We found no history of neurologically tropic infections such as cerebral cryptococcosis, neurocysticercosis, cerebral toxoplasmosis or neurosyphilis. No personal history of depression or anxiety was found. A summary of the distribution of these factors associated with the occurrence of TNC is shown in Table 10 below. (Table 10)
Discussion
To determine the prevalence, clinical presentation and factors associated with the occurrence of neurocognitive disorders in adolescents living with HIV followed up at the CME de la FCB.
Limitations
Our study has some limitations, notably the relatively small size of our sample does not allow us to extrapolate our findings to the general population. The timeframe and period of the study (close to school examinations) did not allow for wider recruitment. Furthermore, our type of study, with no control population, did not allow us to eliminate the effect of certain factors linked to our context. Nevertheless, this is a pioneering study which has enabled us to obtain preliminary results and will provide a better focus for future studies on the same theme.
Socio-demographic characteristics
The sample size was 50 adolescents living with HIV, below the expected number, but still enabling us to obtain pioneering results (compared with 234 in the study by Belete, et al., in Ethiopia [16]). Some adolescents refused to take part, due to the length of the evaluation and examination periods.
Females predominated (68%), reflecting the feminization of the epidemic in sub-Saharan Africa [17,18], although transmission was vertical in most cases.
The 10-19 age group, with the psychological changes typical of adolescence [19-20], made them vulnerable to the risk of developing neurocognitive disorders (NCD).
Various validated tests have been used to assess the various cognitive domains: MoCA [21,22,23], Dubois 5-Word Test [26], Stroop Test, Language Screening Test (LAST) [24], Rey Complex Figure [25].
The prevalence of HANDs was 98% according to MoCA, significantly higher than literature data ranging from 13 to 50% [26-31]. This has been attributed to delayed initiation of antiretroviral therapy and poor compliance [32,33]. Mild forms predominated (78%) ahead of moderate forms (18%), in contrast to studies on adults where mild forms were less frequent [34,35].
Clinical Presentation of Associated Disorders in Our Subjects
Cognitive complaints were present in 70% of adolescents, a higher rate than that found in other studies, such as 27% in Simioni, et al., [34], but close to the 52% of Metha, et al., [35]. This could be linked to the high prevalence of HANDs in this study.
Gnosic, praxic (92%) and working memory (88%) deficits predominated, similar to the 85% memory deficit in Hinkin, et al., [36]. This suggests that HIV affects specific brain regions, compromising school performance.
Inhibitory attention deficits were present in 62% (compared with 32.5% in De Francesco, et al., [37]), reflecting damage to fronto-subcortical structures. 34% suffered from planning disorders (28.9% in De Francesco, et al., [38]), affecting organization and time management. Memory deficit affected 18% of adolescents, less than the 52% reported in adults by Poutiainen, et al., [39], probably due to age and antiretroviral treatment. Finally, 14% had a language deficit, much less than the 60% reported by Brackis-Cott, et al., [40], possibly due to methodological differences.
Advanced HIV infection is associated with a higher prevalence and increased severity of HANDs, as the virus has more time to multiply and affect the brain [41]. Similarly, a prolonged delay before starting effective antiretroviral therapy increases the risk of brain damage. However, despite optimal treatment, HANDs may still occur to a lesser extent [34,42,43]. In this study, 16% of adolescents had developed resistance to antiretrovirals, a recognized risk factor for brain damage [44], although not statistically significant here (p=0.18).
Poor adherence to antiretroviral treatment, which is common in adolescence (58% of cases), favours a drop in CD4 counts and an increase in viral load, thus facilitating viral penetration of the central nervous system. Although other studies have shown a significant link [45,46], this association was not significantly found in this cohort (p=0.42), probably due to the small sample size. Adolescence, however, remains a high-risk period for non-compliance, for a variety of psychological and social reasons [47,48].
Certain antiretrovirals such as Efavirenz, a component of the first-line treatment recommended for children [49,50], have been associated with an increased prevalence of HANDs in previous studies [51]. This may contribute to the high rates observed. A history of malnutrition and opportunistic infections, potential risk factors, could not be precisely assessed in this study.
The abuse of illicit substances such as cocaine (1 case) is known to promote HANDs by increasing viral replication in the brain [52]. However, no statistically significant association was found here (p=0.98), in contrast to the study by Mogambery, et al., [44]. A larger sample size would be required to properly study this factor.
Finally, HANDs can greatly disrupt school learning and may be the cause of the school delays frequently observed in children living with HIV [53,54], up to 3 years behind according to some studies [55,56]. Specific follow-up and support are therefore crucial to prevent these learning difficulties.
Conclusion
This validation study of the MoCA (Montreal Cognitive Assessment) in French-speaking adolescents living with HIV in Cameroon, Central Africa, statistically confirmed the relevance of this tool in this context [57-59].
Internal validation of the MoCA demonstrated its reliability in screening for neurocognitive disorders (NCD) in this population [57]. External validation by comparison with other neuropsychological tests such as the Cognitive Complaints Ǫuestionnaire [58] and the Stroop Test [59] also confirmed the MoCA's ability to identify cognitive deficits.
These results are consistent with previous MoCA validation studies carried out in the French-speaking world, notably in Ǫuebec, Canada [60], France [61], Belgium [62] and Switzerland [62]. They underline the importance of using this simple and rapid tool for the early detection of HANDs in adolescents living with HIV in Central Africa.
After conducting an in-depth study of HANDS in adolescents in our setting, several important conclusions emerged
1) Neurocognitive disorders are a worrying reality: We confirmed the presence of neurocognitive disorders among adolescents living with HIV in our study population. This finding underscores the importance of closely monitoring the cognitive health of this particularly vulnerable population.
2) High prevalence with varied forms: Our study revealed a high prevalence of HANDS, affecting up to 98% of the adolescents included in our sample. These disorders generally presented in mild to moderate forms, suggesting diversity in the severity and manifestation of neurocognitive symptoms.
3) Clinical profile of HANDS: HIV-infected adolescents presented a complex clinical profile, characterized by memory disorders, impaired executive function, and difficulties with praxis and gnosis. These cognitive deficits can have a significant impact on their daily functioning and quality of life.
4) Impact on schooling: We observed a correlation between HANDs and school failure, as well as academic delay. The cognitive difficulties experienced by HIV-infected adolescents can compromise their academic performance, underscoring the importance of integrated management of these aspects of their health.
5) Risk factors identified: Although statistically significant associations were not established, our study identified some potential risk factors for HANDs in these adolescents. These include delayed viral load negativation, often linked to poor adherence or viral resistance to first-line antiretroviral therapy, as well as the use of drugs such as Efavirenz.
In conclusion, our study enabled us to validate the MoCA in French-speaking adolescents in Cameroon, Central Africa. This validation of the MoCA in French highlights the importance of HANDs in our young patients living with HIV. This short scale, quick to administer in a clinical setting, will enable early detection, monitoring and management of neurocognitive disorders in adolescents living with HIV. It is crucial to carry out epidemiological studies with larger samples in this age group of adolescents to better confirm the prevalence of HANDs in this young population, and to better understand these global mental health problems and learning disabilities at school and at work. Strategies for prevention, early detection and treatment of HANDs and co-morbidities will thus be better integrated to improve the quality of life of these young patients, with a view to avoiding academic failure and better preparing them for socio-professional integration.
This study represents the first validation of the MoCA among French-speaking adolescents living with HIV in Central Africa, confirming the reliability and relevance of this tool in this context. However, the relatively small sample size does not allow extrapolation to the entire population. Further, larger-scale studies will be needed to better characterize the prevalence and risk factors of neurocognitive disorders in this age group.
References
- Accessed online at https://www.genscript.com/peptide_assay_failure.html
- Tabb DL, Vega-Montoto L, Rudnick PA, Variyath AM, Ham AJ, et al. (2010) Repeatability and reproducibility in proteomic identifications by liquid chromatography-tandem mass spectrometry. J Proteome Res 9(2): 761-776.
- Tabb DL (2013) Quality assessment for clinical proteomics. Clin Biochem 46(6): 411-420.
- Online accessed at https://www.ema.europa.eu/en/documents/scientific-guideline/draft-guideline-development-and-manufacture-synthetic peptides_en.pdf Draft Guideline on the Development and Manufacture of Synthetic Peptides. EMA/CHMP/CVMP/QWP. 2023.
- Palamutoglu, Recep & sarıçoban, Cemalettin (2019) Physico-chemical investigation and antioxidant activity of encapsulated fish collagen hydrolyzates with maltodextrin. Annals of the University Dunarea de Jos of Galati 43: 94-105.
- Online accessed at https://www.bachem.com/knowledge-center/technical-notes/care-and-handling-of-peptides.
- David V McCalley (2005) Choice of Buffer for the Analysis of Basic Peptides in Reversed-Phase HPLC. Centre for Research in Biomedicine, University of the West of England, Frenchay, Bristol. LCGC Asia Pacific 8.
- Online accessed at https://www.chemeurope.com/en/encyclopedia/Peptide_synthesis.html.
- Martin LJ, Akhavan B, Bilek MMM (2018) Electric fields control the orientation of peptides irreversibly immobilized on radical-functionalized surfaces. Nat Commun 9(1): 357.
- Online accessed at https://www.bachem.com/knowledge-center/technical-notes/care-and-handling-of-peptides.
- Determination of Water Content in Amino acids Using Karl Fischer Titration.
- Li Z, Han X, Hong X, Li X, Gao J, et al. (2021) Lyophilization Serves as an Effective Strategy for Drug Development of the α9α10 Nicotinic Acetylcholine Receptor Antagonist α-Conotoxin GeXIVA [1,2]. Mar Drugs 19(3): 121.
- Hoofnagle AN, Whiteaker JR, Carr SA, Kuhn E, Liu T, et al. (2016) Recommendations for the Generation, Quantification, Storage, and Handling of Peptides Used for Mass Spectrometry-Based Assays. Clin Chem 62(1): 48-69.
- McCarthy D, Han Y, Carrick K, Schmidt D, Workman W, et al. (2023) Reference Standards to Support Quality of Synthetic Peptide Therapeutics. Pharm Res 40(6): 1317-1328.




 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.